Breast Imaging
Breast imaging procedures are a necessity in enabling women and their physicians to maintain thorough breast care . Although medical tests can be nerve-wracking — especially when it comes to waiting for results — they are essential in keeping breasts healthy and getting the patient proper care if breast cancer develops.
The two most commonly used modalities are currently Mammography and Breast Ultrasound.
Mammography
Mammograms are probably the most important tool doctors have not only to screen for breast cancer, but also to diagnose, evaluate, and follow people who’ve had breast cancer. Safe and reasonably accurate, a mammogram is an x-ray photograph of the breast. The technique has been in use for about 40 years.
Mammograms are used as a screening tool to detect early breast cancer in women experiencing no symptoms and to detect and diagnose breast disease in women experiencing symptoms such as a lump, pain or nipple discharge.
Patient Information
Important Things to Know About Mammograms
When to get a mammogram. For now, the recommendation is that women get a mammogram once a year, beginning at age 40. If you're at high risk for breast cancer, with a strong family history of breast or ovarian cancer, or have had radiation treatment to the chest in the past, it's recommended that you start having annual mammograms at a younger age (often beginning around age 30).
They can save your life. Finding breast cancer early reduces your risk of dying from the disease by 25-30% or more. Women should begin having mammograms yearly at age 40, or earlier if they're at high risk.
Don't be afraid. Mammography is a fast procedure (about 20 minutes), and discomfort is minimal for most women. The procedure is safe: there's only a very tiny amount of radiation exposure from a mammogram.
Size does not matter. Although uncommon, breast cancer can also occur in men. Investigation of lumps found in men are done in the same manner as in women, this includes mammography.
Mammography is our most powerful breast cancer detection tool. However, mammograms can still miss 20% of breast cancers that are simply not visible using this technique. Other important tools — such as breast self-exam, clinical breast examination, and possibly ultrasound or MRI — can and should be used as complementary tools, but there are no substitutes or replacements for a mammogram.
An unusual result requiring further testing does not always mean you have breast cancer. About 10% of women (1 in 10) who have a mammogram will require more tests. Only 8-10% of these women will need a biopsy, and about 80% of these biopsies will turn out not to be cancer. It’s normal to worry if you get called back.
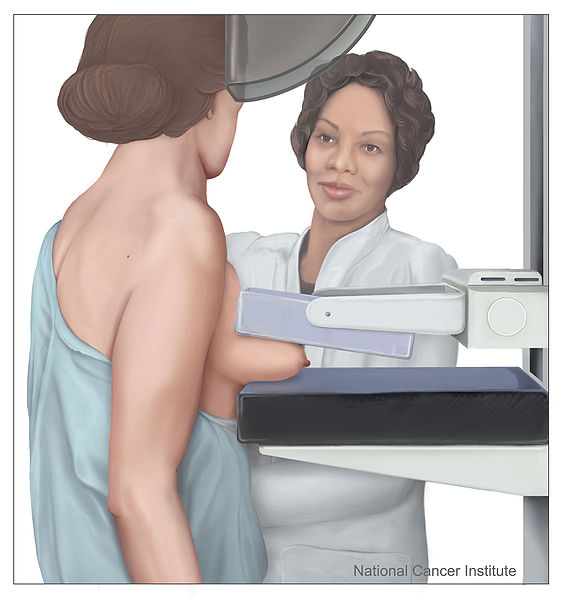
Mammography Technique
When you have a mammogram, a skilled technologist positions and compresses your breast between two clear plates, to even out the breast tissue and to hold the breast still.
The plates are attached to a highly specialized camera, which takes two pictures of the breast from two directions. Then the technologist repeats the technique on the opposite breast. Most screening mammograms include two views of each breast taken from different angles. Diagnostic mammograms involve taking more views than screening mammograms.
For some women, more than two pictures may be needed to include as much tissue as possible.
Deodorant, talcum powder or lotion may show up on the X-ray as calcium spots, and women are asked not to apply these on the day of their investigation.
If you’ve had breast surgery for another reason, such as a benign biopsy or surgery to reduce the size of your breasts, the radiologist will want to know where those scars are in case the scar tissue has to be distinguished from another kind of breast abnormality.
Interventional Mammography
After a screening mammogram, some women may have areas of concern which can't be resolved with only the information available from the screening mammogram. They would then be called back for a "diagnostic mammogram". This phrase essentially means a problem-solving mammogram. During this session, the radiologist will be monitoring each of the additional films as they are taken by a technologist. Depending on the nature of the finding, ultrasound may often used at this point, as well.
Generally the cause of the unusual appearance is found to be benign. If the cause cannot be determined to be benign with sufficient certainty, a biopsy will be recommended. The biopsy procedure will be used to obtain actual tissue from the site for the pathologist to examine microscopically to determine the precise cause of the abnormality. In the past, biopsies were most frequently done in surgery, under local or general anesthesia. The majority are now done with needles using either ultrasound or mammographic guidance to be sure that the area of concern is the area that is biopsied.
Types of breast biopsy procedures include:
- Fine needle aspiration biopsy - a very thin needle is placed into the lump or suspicious area to remove a small sample of fluid and/or tissue. No incision is necessary. A fine needle aspiration biopsy may be performed to help to differentiate a cyst from a lump.

- Core needle biopsy - a large needle is guided into a lump or suspicious area to remove a small cylinder of tissue (also called a core). No incision is necessary.
- Hook-wire needle localization - It is a process which results in inserting a flexible wire beside and beyond the breast lesion pre-operatively to indicate the area of concern to be removed during surgery.
Breast Ultrasound
Ultrasound imaging, also called ultrasound scanning or sonography, involves exposing part of the body to high-frequency sound waves to produce pictures of the inside of the body. Ultrasound exams do not use ionizing radiation (as used in x-rays). Ultrasound imaging of the breast produces a picture of the internal structures of the breast.
How is the procedure performed?
You will lie on your back with your arm raised above your head on the examining table.
A clear gel is applied to the area of the body being studied to help the transducer make secure contact with the body and eliminate air pockets between the transducer and the skin. The sonographer (ultrasound technologist) or radiologist then presses the transducer firmly against the skin and sweeps it back and forth over the area of interest.
When the examination is complete, the patient may be asked to dress and wait while the ultrasound images are reviewed. However, the sonographer or radiologist is often able to review the ultrasound images in real-time as they are acquired and the patient can be released immediately.
This ultrasound examination is usually completed within 30 minutes.
What will I experience during and after the procedure?
Most ultrasound examinations are painless, fast and easy.
After you are positioned on the examination table, the radiologist or sonographer will apply some warm gel on your skin and then place the transducer firmly against your body, moving it back and forth over the area of interest until the desired images are captured. There is usually no discomfort from pressure as the transducer is pressed against the area being examined.
If scanning is performed over an area of tenderness, you may feel pressure or minor pain from the transducer.
If a Doppler ultrasound study is performed, you may actually hear pulse-like sounds that change in pitch as the blood flow is monitored and measured.
You may be asked to change positions during the exam.
Once the imaging is complete, the gel will be wiped off your skin.
After an ultrasound exam, you should be able to resume your normal activities.
Interventional Ultrasound
Ultrasound provides real-time imaging, making it a good tool for guiding minimally invasive procedures such as, needle biopsies (see interventional mammography) and needle aspiration of breast abcesses.
